Never before have the competitive forces for the healthcare premium dollar gathered on the horizon as they have today. Digital-first companies, vertically integrated plans and integrated health systems are competing aggressively to gain more significant market share and profits, especially in the Medicare Advantage segment.
Medicare Advantage plans, or MA plans, as they are commonly referred to, are offered by Medicare-approved private companies that must follow the rules set by Medicare. The federal government pays Medicare Advantage insurers per capita amounts for every covered member and sets limits on out-of-pocket costs for covered services.
With the growth in eligible membership due to an aging boomer population, MA is an attractive investment segment. National health plans have primarily served this segment, such as United Health Group (UHG), Anthem and Humana, as well as various regional Blue Cross Blue Shield (BCBS) community health plans. But a new breed of digital health startups, including insurtech companies and technology innovators offering point solutions, are now targeting MA.
The federal government updates MA payments through a complex formula based on how spending fluctuates in the traditional Medicare program and other factors. With the Biden administration’s announcement of a substantial rate hike in 2023, increased interest in the MA population segment leads to a highly competitive landscape.
We are seeing the rise of digital-first companies such as Devoted Health, which has raised nearly $ 2 billion in venture capital, targeting the MA population. Hospitals are trying to become insurers as well. Traditional health systems, including one of my clients, Prisma Health, are launching brand-new health plans targeting the MA population. The Healthcare Finance Management Association (HFMA) and consulting firm Guidehouse found that “ nearly 60% of health systems plan to advance into risk-based Medicare Advantage models in 2022.”
Managing The MA Business
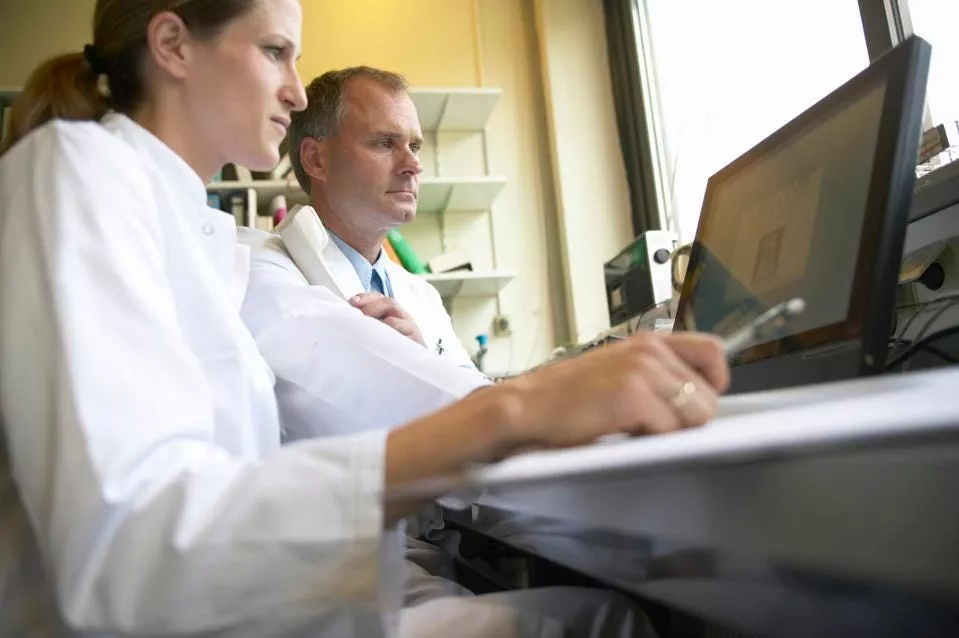
The big focus for all the players in the MA ecosystem has been on controlling medical costs. Large health plans such as UHG and Humana have adopted a strategy of vertical integration to gain more control over medical expenses for their covered population. In this vein, UHG has bought 10,000 clinician practices in the past few years; Humana owns over 200 clinics and has invested in home healthcare. These organizations are also building solid foundations in data and analytics, leveraging data on their member populations and, in some cases, acquiring them, as is the case with the pending acquisition of Change Healthcare by UHG.
New insurtech providers like Oscar, Clover and Bright Health are approaching the market from a digital-first, data-enabled perspective. Lacking a heritage in healthcare services, they are also running into challenges. Clover Health, which went public in a SPAC transaction, lost more than $4,500 per member in 2021 , which translates to a 100% medical loss ratio. In other words, they spent all their premium dollars on medical expenses bills for members. Bright Health has pulled out of several states citing high medical costs from unexpected pandemic-related expenses.
The Role Of Digital Platforms And Experiences
The ability to provide engaging digital experiences, supported and enabled by advanced data analytics in order to improve access and care, is emerging as the most critical strategic differentiator for health plans—especially those focused on the MA segment.
Large health plans such as Humana, UHG and Anthem have elevated the digital function to be the face of strategic capabilities that define a vision for the future of enterprises. They are focusing on personalized consumer experiences, provider enablement and advanced analytics. Ten years ago, I switched doctors because my PCP had no tolerance for anything digital, and he would not use the EHR system. Today, patient portals are table stakes, and over 60% of respondents in an Experian Health and Pymnts survey indicated they would switch to a healthcare provider that has one. Indeed, visiting a doctor today can be entirely a digital experience.
Another reason for the enhanced focus on digital experiences is the rating program for Medicare rewards health insurers who provide superior experiences. Members often use Medicare Star Ratings to select their health plans, and higher ratings translate directly into market share gains through new member acquisitions. Consulting firm McKinsey estimates that “with the latest changes … customer experience will account for approximately 57 percent of overall Star Rating in 2023.”
At the other end of the spectrum, integrated health systems, also known as payviders (providers who also own a payer or health plan), are uniquely positioned to take advantage of the Medicare Advantage opportunity. My work with a payvider has provided deep insights into how members and patients can be targeted effectively for healthcare services campaigns, health risk management and superior online experiences.
Payer-Provider Collaboration As The Way Forward
As healthcare moves forward, driven by consumerism and technology enablement, healthcare organizations must focus not just on getting the experience right but also on collaborating with others in the ecosystem to improve risk-management capabilities and manage costs. Payer-provider collaboration holds the key. Leading healthcare organizations are embracing unusual and creative partnerships with technology firms and other healthcare enterprises to reach these goals.
One example is leveraging a common CRM platform across health plans and clinical enterprises in order to help you understand and engage with members within the integrated health system. Pooling data across enterprises is another method to embrace partnerships. Examples include Anthem’s partnership with EHR vendor Epic to deliver prior authorizations and other meaningful information directly into provider workflows. There is also Highmark Insurance’s 10-year partnership with ChristianaCare to use shared data to improve health outcomes. As the competition for the MA premium dollar intensifies, it will require breaking boundaries to achieve breakthrough performance.